Giving our patients the information and understanding that they need can be a powerful tool in shaping positive health behaviours. As physiotherapists, we often use education as a way to do this alongside other modes of treatment. In this page we have provided with some tips and suggestions to optimise your patient education skills both in the virtual and the real world.
- Many people search online for information about their health condition
- There are two important components to education via telehealth:
- Educate the patient about telehealth (e.g. expectations, value, benefits and shortcomings of telehealth)
- Educate patient about their condition and options for self-management strategies.. This paper highlights providing education or information as a crucial component of best practice care for musculoskeletal pain.
- Integrate the use of online resources to re-enforce key messages. See Patient Links for examples.
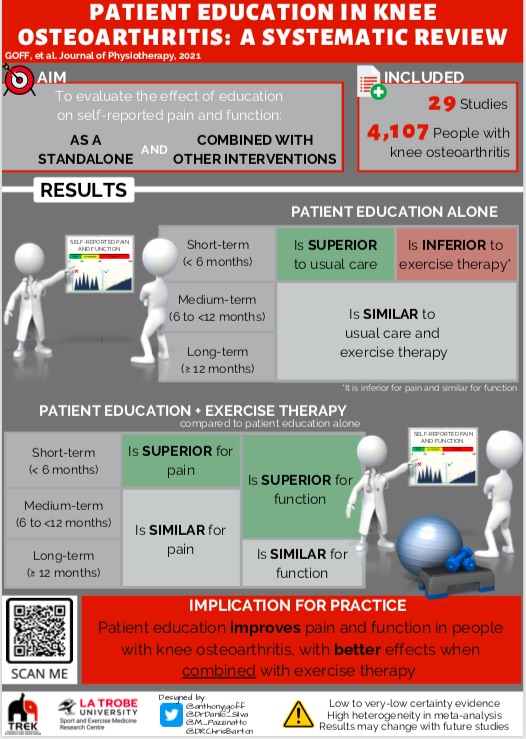
Have a look at the infographic below to learn more about the evidence on the effectiveness of education on patient outcomes.
Key tips
- Education alone is has limited effectiveness. You need to understand your patients’ beliefs, learning needs, and readiness for behaviour change.
- Don’t just ‘information dump’ – you need to customise the information to your patient and adapt to their level of health literacy and understanding.
- Reflect (repeat back to patient) key thoughts from their subjective assessment (e.g. it sounds like you are worried that exercise will damage your knee)
- Ask and understand your patients’ beliefs (i.e. high impact exercise will cause further damage to my knee), then provide evidence that contradicts these beliefs (i.e. runners have lower risk of osteoarthritis than non-runners)
Changing the Narrative
Read this paper on changing the narrative about knee osteoarthritis care. Despite the paper having a specific population, the principles are still applicable to other musculoskeletal conditions.

The take home messages from this paper are:
-
Change the message (e.g. pain is a modifiable symptom related to sensitised structures and influenced by many biopsychosocial factors)
-
Change the treatment focus from structural damage to modifiable biopsychosocial factors
-
Put the patient in charge of their own care by using a self-management approach.
Next – Adjunct Therapies
